State Opioid Response (SOR)
Detroit Wayne Integrated Health Network was awarded State Opioid Response funding in 2019 as a measure to reduce overdose deaths related to opioids in Michigan which are of epidemic proportion. The State Opioid Response Grant is a comprehensive program constructed to combat to the surge of opioid related overdoses tailored to encompass prevention, treatment and recovery services, the first grant of its kind to target all facets of SUD services. Prevention services have a two-tier approach to prevent the onset of addiction in high risk population groups, and to prevent fatal overdoses through the distribution of naloxone. Treatment services address the onset and progression of opioid use disorder, designed to help the individual progress to remission. Recovery programs are designed to empower and engage individuals in recovery and prevent relapse.
Programs:
Evidence Based Prevention
Programs funded under this project will have evidence of effectiveness in preventing opioid misuse and opioid dependence or opioid deaths. Prevention providers will select from the 4 evidence-based practices (EBPs) established by MDHHS. These EBPs have evidence of the effectiveness of preventing illicit drug use in middle school and high school age youth. Therefore, SOR prevention funds will be used to implement Botvin LifeSkills, Prime for Life, Guiding Good Choices, Strengthening Families, and Project Toward No Drug Abuse.
Overdose Education and Naloxone Distribution Programs
.jpg) Prevention providers will order Narcan through the MDHHS portal or DWIHN’s inventory. The providers will use SOR III funds to sustain and enhance efforts to distribute naloxone to law enforcement, corrections, faith-based organizations, barber shops, salons, bars, hotels, restaurants, and in some instances, known drug houses. To enroll, the providers must receive initial overdose recognition and response training from DWIHN’s SOR Coordinator (Matt Yascolt), SUD Director (Judy Davis), or the Prevention Manager (Karra Thomas). They will operate under a naloxone standing order to distribute free take-home kits directly to individuals, friends, and family members at risk of experiencing an opioid overdose. In addition, they will be able to fund other harm reduction activities, including but not limited to infectious disease education, immunizations, naloxone training and distribution, purchase and distribution of fentanyl test strips, Nalox-Boxes, PPEs, and universal precaution supplies. Participating providers will submit monthly reports to DWIHN documenting the number of Narcan kits and fentanyl test strips distributed and the number of overdose reversals reported.
Prevention providers will order Narcan through the MDHHS portal or DWIHN’s inventory. The providers will use SOR III funds to sustain and enhance efforts to distribute naloxone to law enforcement, corrections, faith-based organizations, barber shops, salons, bars, hotels, restaurants, and in some instances, known drug houses. To enroll, the providers must receive initial overdose recognition and response training from DWIHN’s SOR Coordinator (Matt Yascolt), SUD Director (Judy Davis), or the Prevention Manager (Karra Thomas). They will operate under a naloxone standing order to distribute free take-home kits directly to individuals, friends, and family members at risk of experiencing an opioid overdose. In addition, they will be able to fund other harm reduction activities, including but not limited to infectious disease education, immunizations, naloxone training and distribution, purchase and distribution of fentanyl test strips, Nalox-Boxes, PPEs, and universal precaution supplies. Participating providers will submit monthly reports to DWIHN documenting the number of Narcan kits and fentanyl test strips distributed and the number of overdose reversals reported.Peer Outreach and Linkage Programs
The project will implement Peer Recovery Coach services in outpatient settings such as FQHCs, Urgent Care, Eds, shelters, etc. Peer Recovery Coaches will provide referrals within these outpatient settings or individuals presenting with an OUD or Stimulant Disorder. An SBIRT model will be applied upon assessment to determine if a referral to treatment or recovery services is necessary. In addition, the coaches will require follow-up on referred individuals within 30 days to assess the need for additional services and peer support. QRT- Peer Recovery Coaches (PRC) will engage with individuals within 24 to 72 hours, build trust, understand their needs and desires, and connect them with services that decrease the risk of future overdose mortality, including naloxone harm reduction programs or substance use disorder treatment. In addition, the EBP, Motivational Interviewing client-centered approach to inspire clients in resolving ambivalence toward treatment has proven to be an effective tool in developing trusting relationships with staff and members. The program will support Wayne County residents and implement timely communication, care, coordination, risk reduction, and other overdose prevention interventions. The PRCs will work closely with law enforcement agents and health departments to monitor high-risk areas for overdose. The trained PRCs will also train healthcare professionals and law enforcement to support opioid rapid response efforts, including linkages to care and gap care.
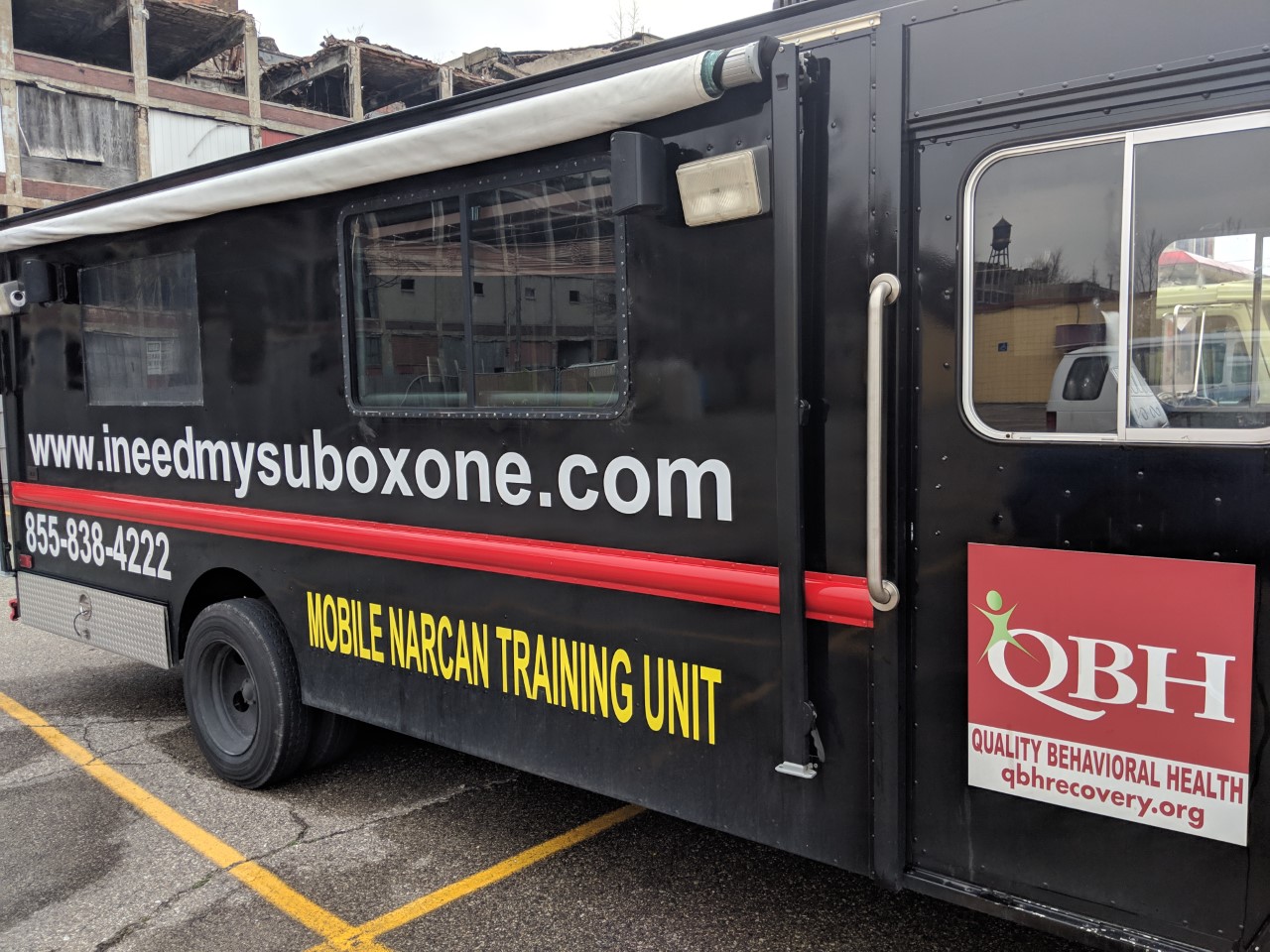
Mobile Care Unit Programs
Mobile triage units will implement services for transient individuals with a substance use disorder. The services will consist of street-based outreach to active OUD and stimulant users. This will also include reimbursement for insurance for the mobile units, staff, supplies, and medication. The mobile units will be retrofitted vans/buses that will bring counseling, therapeutic and physical health services to individuals. In addition, the units will have an area for intake and scheduling, a restroom that incorporates urine screening, and at least one private counseling area.


Opioid Use Disorder and Stimulant Use Disorder Programs
The grant programs will provide funding to expand access to OUD prevention, treatment, and recovery support services. Within this broad mandate a projected 300 uninsured and underinsured individuals will receive direct treatment services for OUDs in Wayne County. Services may include case management and OHH services, individual, group, and transportation and can be in a 24- hour setting. Providers will be required to collect GPRA data as well.
Recovery Housing Programs
Providers will increase access to recovery supportive housing. These efforts will include implementing additional recovery housing units for both men and women and pregnant women and parents with children. Measures will also include a rapid re-housing model to provide rental assistance, application fees, deposits, and utility assistance to individuals with OUD or stimulant use disorder who have limited income for safe and secure housing.
GPRA is the Government Performance Results Act. Any client receiving SOR-funded treatmentand/or recovery services is required to complete three interviews at specific time-points:
- Intake – occurs within 24 hours of receiving first SOR-funded services;
- Discharge – occurs on last day client received SOR-funded services;
- 6-month follow-up – occurs between 5 months and 8 months post-Intake interview date
Click HERE for Provider link to GPRA: Recipients should enter their data within 1 day—but no later than 7 days—after the GPRA interview is conducted
Note: GPRA is required for all recipients of SOR 3 treatment and recovery programs. Programs included: Recovery Homes, Jail-based MAT, and OUD/StUD Treatment.
SOR Coordinator:
Matt Yascolt: myascolt@dwihn.org
SUD Director:
Judy Davis: jdavis@dwihn.org
Prevention Manager:
Karra Thomas: kthomas@dwihn.org
